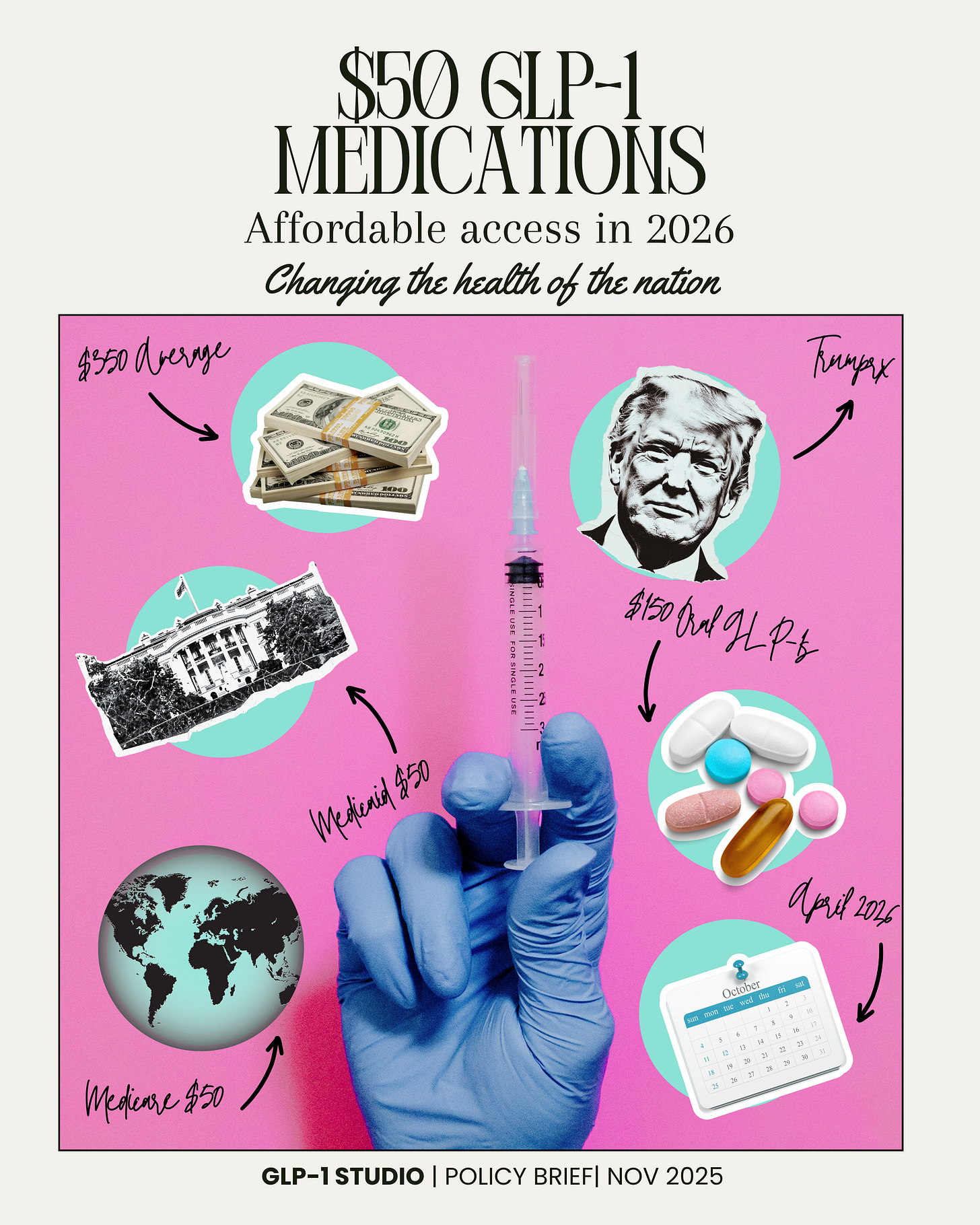
The Biggest Announcement in GLP-1 Patient History
Affordable access to GLP-1 medications
Nov. 6th, the White House made an announcement that could potentially reshape the health of our entire nation.
As if the announcement itself wasn’t big enough, the way the news dropped and who I was with, made it that much more of a whirl.
The Announcement
The White House confirmed new pricing agreements with Eli Lilly and Novo Nordisk under the federal TrumpRx program.
This new agreement brings the list price for brand name GLP-1 medications like: Ozempic, Wegovy, and Zepbound down to Most-Favored-Nation (MFN) levels, finally putting Americans on par with what other countries pay.
For the first time ever, Medicare and Medicaid will cover these drugs for obesity—and with only a $50 co-pay!
Now that list prices are finally being standardized across the board, I’m hopeful that commercial insurers will follow suit and expand access for people who are above the federal poverty line but still struggling to pay for their medications out of pocket.
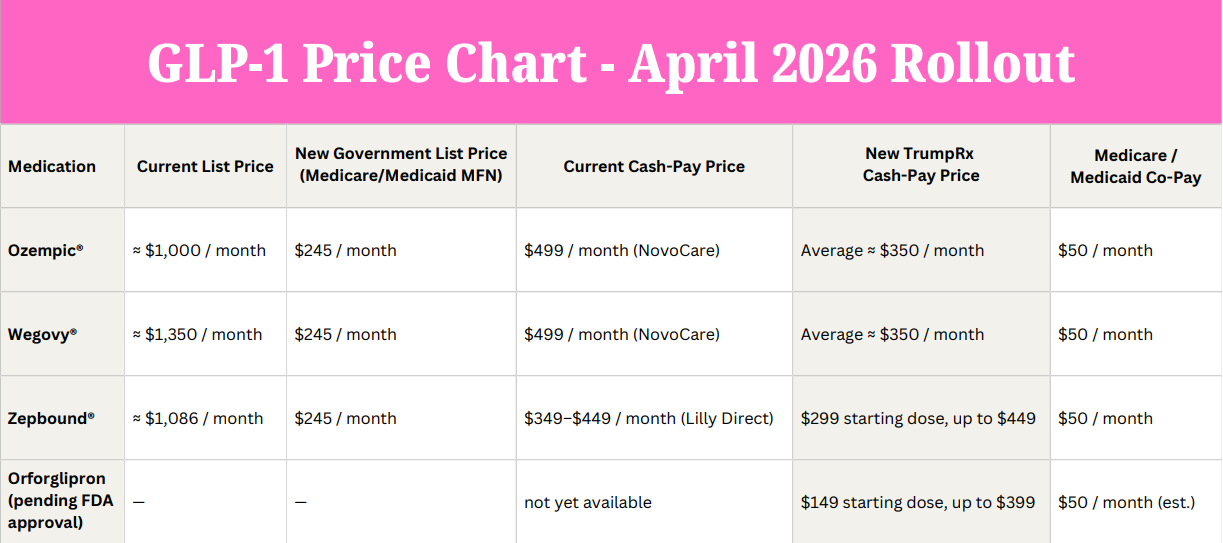
Price Breakdown
Here’s What’s Changing for GLP-1 Medications:
Most-Favored-Nation (MFN)
The U.S. has been paying some of the highest medication prices in the world because drug companies could charge whatever they wanted.
Same medicine, but in other countries, people pay only a fraction of the cost.
MFN pricing is a new rule that says, If other countries get a lower price, we should get that price too.
TrumpRx
TrumpRx is a list of fair prices. This list shows how much certain drugs, like Ozempic or Wegovy, should really cost.
It’s not a pharmacy or a discount card. It’s more like a rulebook that keeps prices fair.
Before this system, people couldn’t really see what medicines were supposed to cost. Every pharmacy and insurance company had different prices, and most of it was a secret.
Now, with this new system, everyone can finally see the actual price. It makes the cost fair and clear, so no one in the U.S. pays more than people in other countries for the same medicine.
Think of Most-Favored-Nation pricing as the government’s version of a “price-match guarantee.” If another wealthy country gets a better deal on a drug, the U.S. automatically gets that deal too. Pharmacy Benefit Managers (PBMs)
PBMs are the middlemen who sit between drug companies, insurance plans, and pharmacies. They’ve had a huge influence on drug prices — often driving costs up so they can take a bigger cut.
Here’s what this new system could mean for them:
Less secrecy: Prices are public and fixed, so no more hiding behind rebate deals.
Smaller profits: Slimmer price margins take away their biggest source of extra revenue.
Less control: The federal price list sets a ceiling they can’t inflate.
More accountability: With less room for hidden markups, PBMs will face growing pressure to show how they actually save money.
PBMs have long helped keep prices high because the system rewarded them for it. The new TrumpRx and MFN plan could finally shine a light on how the system really works and make medicine prices clear instead of marked up.
What This Means for Patients
This announcement is massive and it’s going to touch so many lives in so many different ways.
With this policy in place, it means:
Recognition: Obesity care is now seen as essential medical treatment, not elective or cosmetic.
Medicare: Coverage will finally include obesity medications, giving millions of older adults new access.
Medicaid: Programs in all 50 states can offer coverage with a $50 copay for those under the federal poverty line.
Prescribing: Doctors may be more willing to recommend GLP-1s as cost and coverage barriers disappear.
Cash-pay: Patients paying out of pocket may not see big changes yet, but coverage expansion is the goal.
Commercial: Private insurers often follow once Medicare and Medicaid set the standard.
Validation: GLP-1s are now seen as a public-health tool, not a luxury.
When these medications first came to market, they came with eye-watering $1000+ price tags. Most people, even those with insurance, couldn’t begin to afford that.
Now, with MFN pricing and public coverage, the wall between “who can afford treatment” and “who can’t” is finally starting to come down.
“…to ensure the American healthcare system is promoting health and addressing the root causes of chronic disease.”
What This Means to Me
For the past year, I’ve poured everything I have into affordable access.
It’s been equal parts passion and exhaustion, doing a thousand little things that sometimes felt like they barely made a dent.
I started petitions (Change.org and Sway), launched a Podcast, founded a nonprofit, wrote letters to the FDA (seen here and here) and USPTO, organized Contact Congress Day, connected patients with reporters and organizations, and shared their stories with anyone who would listen.
Somewhere along the way, GLP-1 Studio grew into a full-blown media production—a home for me and a lifeline for people searching for hope.
So when I heard the words “Medicare and Medicaid will cover GLP-1s for obesity,” I think of the thousands of people who’ve shared their stories with me: those who rationed doses, sold belongings, or went without entirely, and it brings me to tears.
I’ve lived that reality too.
Watching this announcement, while standing shoulder to shoulder with other advocates, and a Danish documentary crew filming us, felt completely surreal, like watching history unfold in real time.
At its core, my goal has always been: affordable access for anyone who needs it.
The truest version of that is real coverage, with a fair copay. There’s still work to do, but for the first time, the future we’ve been fighting for is finally beginning to take shape.